Section 4: Intervention thresholds and strategy
Recommendations
- An initial FRAX assessment, which provides the ten-year probability of a major osteoporotic fracture (MOF; clinical spine, hip, forearm or humerus) and/or hip fracture, can be used to identify patients at low, intermediate, high or very high risk of fracture (Strong recommendation).
- Consider, particularly in older people, drug treatment in those with a prior and/or recent fragility fracture, with fracture risk assessment informing the choice of drug treatment (Strong recommendation).
- Men and women with high and very high fracture risk ( see Figure 1) should have a DXA if a baseline measurement is needed against which to compare future BMD measurements (Strong recommendation).
- Men and women with intermediate fracture risk (i.e., between the upper and lower assessment thresholds) should be referred for BMD measurement, if practical. Thereafter, fracture probability should be reassessed using FRAX (Strong recommendation).
- When BMD is included in a FRAX assessment, the patient’s risk (high, very high or low) is determined by the higher of the two (MOF and hip fracture) risk assessments (Strong recommendation).
- In men and women with intermediate fracture risk, if BMD measurement is unavailable, contraindicated, or impractical (e.g., in frail individuals), drug treatment should be offered if there is a history of fragility fracture and/or if fracture risk exceeds the intervention threshold (Strong recommendation).
- Men and women with low fracture risk, without a prior fragility fracture, can be reassured that their fracture risk is low and offered lifestyle advice as appropriate (Strong recommendation).
-
Consider referral of very high-risk patients to an osteoporosis specialist in secondary care, for assessment
and consideration of parenteral treatment (some may need first-line anabolic drug treatment, especially
those with multiple vertebral fractures). Indications of very high risk, where specialist referral should be
considered include (Conditional recommendation):
-
The presence of single but important clinical risk factors, such as,
- A recent vertebral fracture [within the last 2 years]
- ≥2 vertebral fractures [whenever they have occurred]
- BMD T-Score ≤-3.5
- Treatment with high dose glucocorticoids [≥7.5 mg/day of prednisolone or equivalent over 3 months] (refer urgently given rapid loss in bone post initiation of glucocorticoids; if any delay is anticipated, start an oral bisphosphonate in the meantime)
- The presence of multiple clinical risk factors, particularly with a recent fragility fracture indicating high imminent risk of re-fracture,
- Or other indicators of very high fracture risk, including as defined by FRAX.
-
The presence of single but important clinical risk factors, such as,
- The choice of drug treatment should be informed by the level of fracture risk, additional clinical risk factors, cost-effectiveness of treatment and patient preferences (Strong recommendation).
- FRAX and the link to the NOGG website should be incorporated into electronic patient health record systems (Strong recommendation).
FRAX assessment thresholds for ten-year probability of fracture
-
The approach recommended for decision-making is based on fracture probabilities derived from FRAX and can be
applied to men and women 78. This approach is
underpinned by cost-effectiveness analysis with oral or intravenous bisphosphonates as the intervention
116,117;
(Evidence level Ib). FRAX assessment thresholds for ten-year probability of a major osteoporotic
fracture (MOF) are shown in Figure 1.
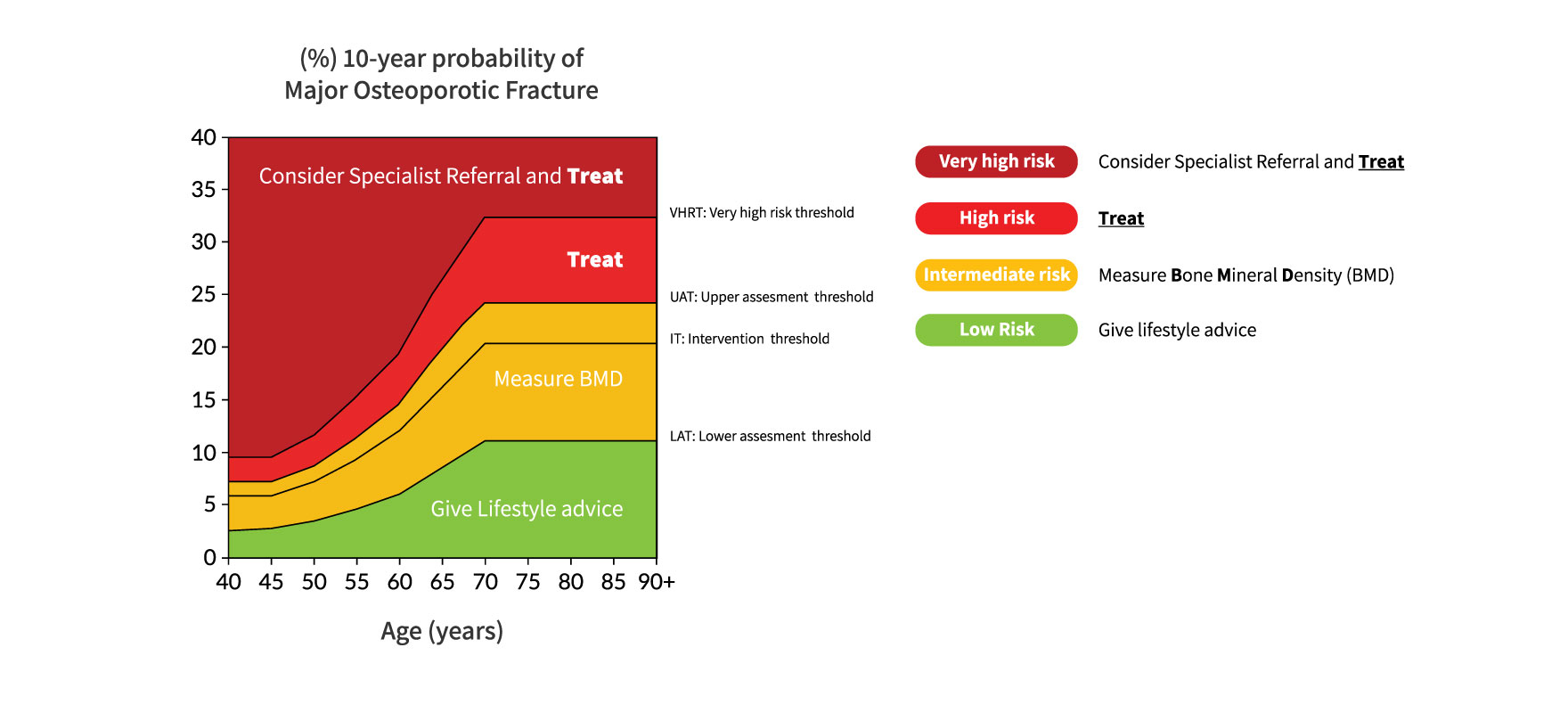
Figure 1: NOGG assessment, intervention and risk thresholds for major osteoporotic fracture probability (MOF) in the UK with the use of FRAX. Individuals with probabilities below the lower assessment threshold (LAT) are considered for lifestyle advice. Those at intermediate risk (probabilities between the upper assessment threshold (UAT) and lower assessment threshold (LAT) are further assessed with BMD measurement. Where probabilities calculated using BMD lie above or below the intervention threshold (IT), treatment or lifestyle advice, respectively, is recommended 3,78. Patients with probabilities above the upper assessment threshold (UAT) are considered for treatment. Those with probabilities above the very high-risk threshold (VHRT) should be considered for specialist referral. Where BMD measurement is not practical (e.g. when individuals are frail and unable to get onto a DXA table, or lie flat on a DXA table), patients with probabilities above the IT are considered for treatment.
- The use of FRAX without BMD has approximately the same performance as BMD without FRAX 11; (Evidence level Ia). Thus, the same intervention threshold can be used when fracture risk is assessed with or without BMD (see Figure 1).
- For men and women, the intervention threshold up to age 70 years is set at a risk equivalent to that of a woman of the same age with a prior fracture, in line with current clinical practice, and therefore rises with age. At age 70 years and above, fixed thresholds are applied 118; (Evidence level Ib). The proportion of women potentially eligible for treatment rises from approximately 30% to 50% with age, largely driven by the prevalence of prior fracture 118; (Evidence level Ib).
- When FRAX is calculated with BMD included, the NOGG website also provides intervention thresholds based on the 10-year probability of hip fracture, in addition to the 10-year probability of a MOF (Figure 2). If there is discordance between the risk categories identified by the two probabilities, the highest risk category can be used to guide intervention. Of note, in the SCOOP study of screening for high fracture risk, treatment was targeted on the basis of risk assessed by hip fracture probability, with or without BMD 119.
Indications for specialist referral in those at very high fracture risk
- Individuals at very high fracture risk have the most to gain from thorough investigation of osteoporosis, falls assessment, and development and delivery of a personalised treatment plan for a chronic, life-long condition. A range of treatments now available to treat osteoporosis are mostly (but not exclusively) initiated through secondary care ( see Section 6), and the sequence in which they are used is important. Three anabolic agents (teriparatide, abaloparatide and romosozumab) are now available, with teriparatide licensed for a once only treatment course. Within the licencing permissions all anabolic agents might be used at different stages within the course of a lifetime of osteoporosis; however, there is currently no evidence to support a specific sequence and input from an osteoporosis specialist is essential to inform a personalised care plans (see Section 6).
- Treatment with teriparatide or abaloparatide, which are anabolic skeletal agents, or romosozumab which has a dual anabolic and antiresorptive action, result in rapid and greater fracture risk reductions than some antiresorptive treatments ( see Section 6) 120-122, 123;(Evidence level Ib). This has led to the need to identify the sub-group of patients at very high fracture risk who would potentially benefit from clinical review by an osteoporosis specialist, and who may benefit from anabolic drug treatment 124.
- Indications for referral to an osteoporosis specialist may arise through several routes, for example in the presence of single but important clinical risk factors, such as a recent vertebral fracture [within the last 2 years], ≥2 vertebral fractures [whenever they have occurred], a BMD T-Score ≤-3.5, high dose glucocorticoids use (≥7.5 mg/day of prednisolone or equivalent over 3 months) (see Section 7) 55, 125; (Evidence levels IIb and IV), or via a combination of clinical risk factors, resulting in very high fracture risk 126; (Evidence level IIb).
- Prior fragility fracture is a well-established risk factor for a future fracture. This risk of subsequent osteoporotic fracture is particularly acute immediately after an index fracture and wanes progressively over the next 2 years, but thereafter remains higher than that of the general population 103,127-134 . This effect of recency of fracture, sometimes termed imminent risk 133, is also dependent on age, sex and site of fracture 52; (Evidence level Ic). This complexity is being addressed by the development of optional post-FRAX algorithms to allow clinicians to explore the potential impact of fracture recency on the calculated probability of MOF and hip fracture (see Table 2) 52. The mechanism underlying imminent risk is not yet fully understood and no clinical risk factors have yet been identified for short term recurrent fractures that differ from those identified for fracture over a longer time horizon 77. Few therapeutic studies have reported the recency of fracture in those patients whom they have recruited, though rapid clinical efficacy has been demonstrated within studies of zoledronate, risedronate, teriparatide, abaloparatide and romosozumab 121,135, 136,123; (Evidence level Ib).
- A NOGG threshold that characterises men and women at high and very high fracture risk has also been established using FRAX probabilities; very high risk is identified as a FRAX-based fracture probability that exceeds the intervention threshold by 60% (Figures 1 and 2) 137. It can be used to identify patients who likely require specialist referral for assessment of their osteoporosis (which should include DXA measurement of BMD), and further consideration of appropriate treatment strategies 124,138 . The proportion of postmenopausal women at very high risk defined in this way rises from approximately 6% at age 50-54 to 36% at age 90 years or older. Numerical values for the probability thresholds are given in Table 5 for MOF and for hip fracture. An assessment algorithm is shown in Figure 3.
- In patients with FRAX probabilities in the high-risk category,
consideration of
additional clinical risk factors (e.g., frequent falls, very low spine BMD – see Table 2) can also lead to
redesignation from high to very high risk of fracture.
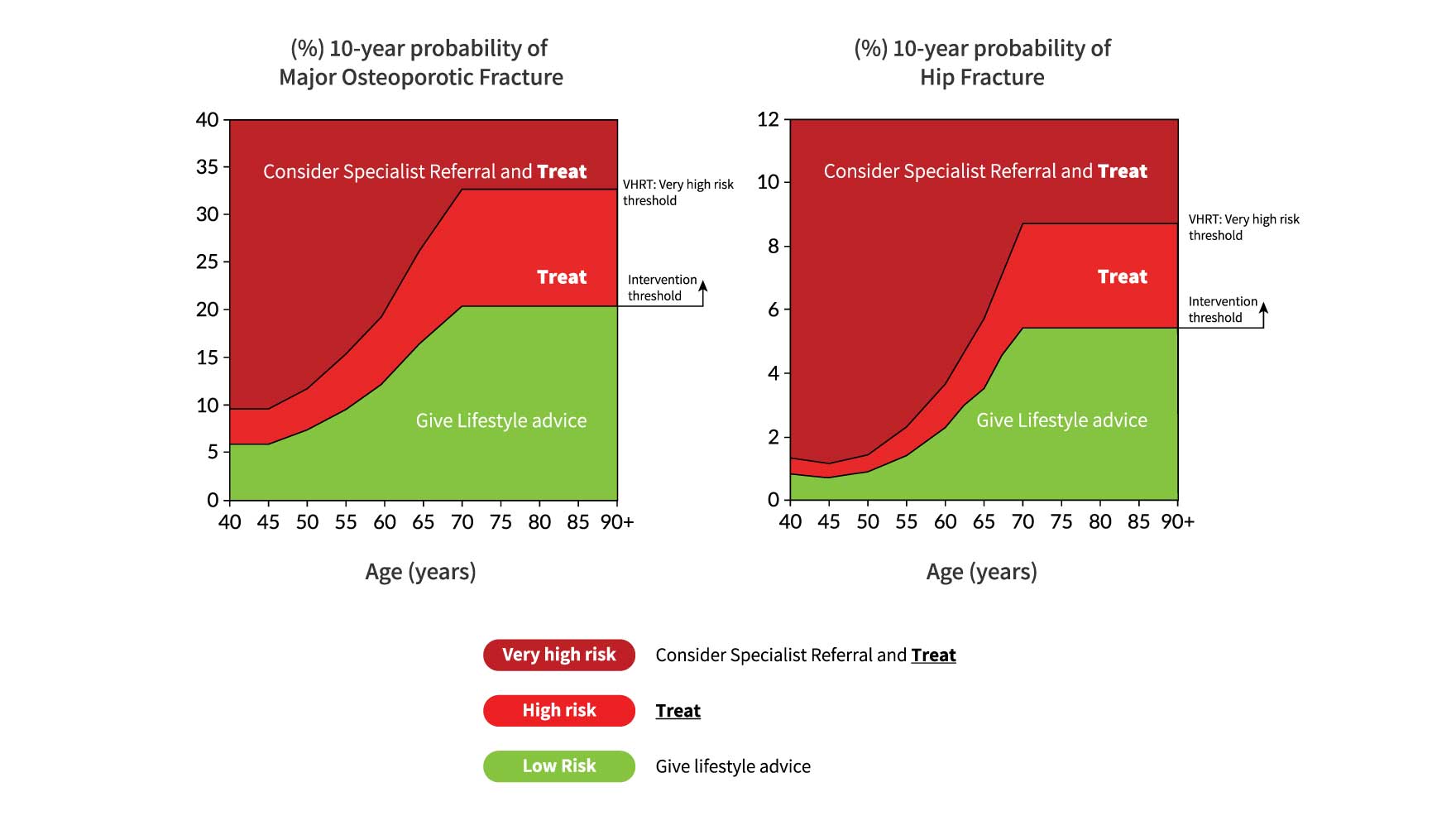
Figure 2: NOGG thresholds for intervention and/or referral using major osteoporotic fracture (MOF) and hip fracture (HF) probabilities in the UK. The panels show the thresholds following the recalculation of FRAX after the input of BMD; the same thresholds are used when BMD is unavailable. The intervention threshold (IT) and very high-risk threshold (VHRT) denote the thresholds for high and very high risk, respectively.
Table 5: Numerical values for NOGG thresholds for major osteoporotic fracture and hip fracture probabilities based on FRAX. LAT and UAT refer to the lower and upper assessment thresholds, respectively, between which a BMD is indicated. The intervention threshold (IT) and very high-risk threshold (VHRT) denote the thresholds for high and very high risk.Age (years) LAT IT UAT VHRT Major osteoporotic fracture 50 3.4 7.3 8.8 11.7 55 4.5 9.5 11.4 15.2 60 6.0 12.2 14.6 19.4 65 8.6 16.5 19.8 26.4 70 11.1 20.3 24.4 32.5 Hip fracture 50 0.23 0.91 1.1 1.5 55 0.43 1.5 1.7 2.3 60 0.80 2.3 2.8 3.7 65 1.4 3.5 4.2 5.6 70 2.6 5.4 6.5 8.6 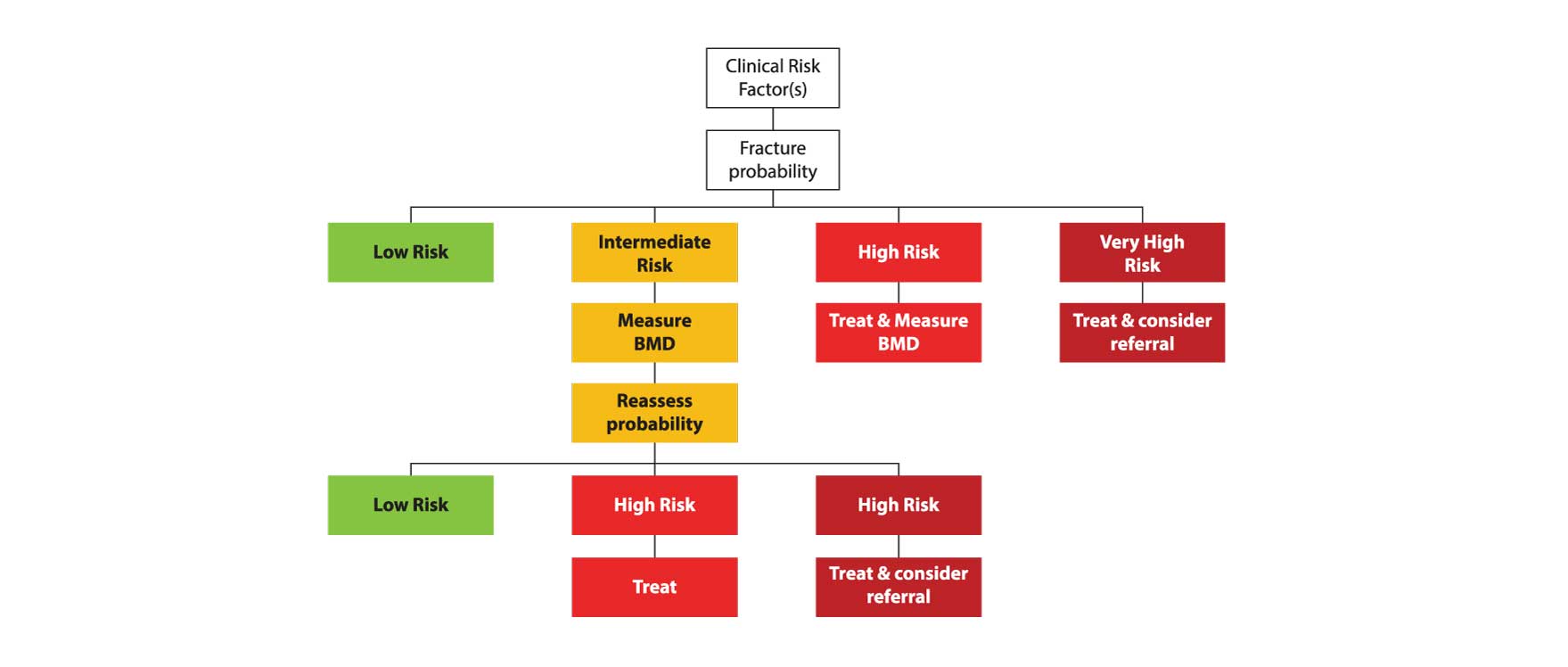
Figure 3: Management algorithm for the assessment of individuals at risk of fracture 137. Those at very high risk should be treated and considered for referral to an osteoporosis specialist in secondary care; some may benefit from parenteral treatment (including first-line anabolic drug treatment, especially if multiple vertebral fractures). All individuals should be offered lifestyle advice. CRF: Clinical Risk Factor.
- The FRAX MOF probabilities are transferred automatically to the NOGG website, by clicking on the specified button on the FRAX results box. Where practitioners receive the results of a FRAX risk assessment for an individual patient without treatment guidance, the FRAX probabilities can also be entered manually onto the NOGG website ( https://www.nogg.org.uk/manual-data-entry); this page also captures additional information (age, sex, glucocorticoid exposure and finally, whether a femoral neck BMD has been included, in the FRAX estimates) so that the result can be automatically compared to the NOGG thresholds with appropriate guidance on treatment.
- In the case of a patient born in another country, now living in the UK, FRAX-derived probabilities from a non-UK FRAX tool can be entered manually onto the NOGG website ( https://www.nogg.org.uk/manual-data-entry), to determine where risk lies in relation to intervention thresholds.
- Lack of integration of FRAX assessments and links to NOGG guidance in existing patient health record systems represents a barrier to effective fracture risk assessment (Evidence level IV).
- The targeted use of BMD assessments with the NOGG strategy makes more efficient use of often limited resources than would DXA scanning of all individuals with risk factors 139; (Evidence level Ib). Historically it was thought that treatment should not be undertaken in women without initial BMD measurement, except in those with hip or vertebral fractures. This view arose after a post-hoc analysis in 1998 suggested reduced efficacy of alendronate in patients with BMD T-scores above -2.5 140; (Evidence level Ib). However, this approach is now outdated as many studies have since shown little or no interaction of BMD on the effectiveness of several agents, including bisphosphonates (e.g., zoledronate, denosumab, raloxifene, abaloparatide and teriparatide) 63, 141-144, 145-146; (Evidence level Ib). Moreover, clinical risk factors are not totally independent of BMD and, when clinical risk factors alone are used in women age 70 years or more to identify patients at high fracture risk, BMD is approximately 1SD lower in the high-risk group compared with a low-risk group 147 ,148; (Evidence level Ib). These findings indicate that the categorisation of patients at high fracture risk on the basis of FRAX without BMD mostly selects patients with low BMD and that the higher the fracture probability, the lower the BMD. Note that this does not preclude the use of DXA scanning if more widely available; in addition to providing the most accurate risk assessment, DXA provides a baseline measurement for treatment monitoring and also permits, again if available and indicated, detection of vertebral fractures using VFA ( see Section 3).
- FRAX is not recommended as a tool to monitor treatment 149; (Evidence level IIb). However, the use of FRAX is appropriate to re-evaluate current fracture probabilities when considering a change in patient management; (Evidence level IV).